Facial Animation Laboratory
Welcome to the Facial Animation Laboratory! Thank you for taking the time to learn more about our exciting research and our state-of-the-art methods for collecting important data to help individuals diagnosed with Facial Paralysis and Cleft Lip and Palate. Find out more information below, or learn more on the Facial Animation Laboratory's website.
About the Lab
The Facial Animation Laboratory team at Tufts University School of Dental Medicine is currently working on two federal grants, both funded by the National Institute of Dental and Craniofacial Research. Principal Investigator, Dr. Carroll Ann Trotman, is investigating two major craniofacial issues: facial paralysis and cleft lip and palate surgery. Located at 75 Kneeland Street in downtown Boston, we collect extensive data on patients diagnosed with acute Facial Paralysis and patients with Cleft Lip and Palate using three-dimensional imaging equipment.
The focus of the research conducted in the Facial Animation Laboratory is on the development and use of objective measures to assess outcomes of soft tissue surgeries and the recovery process for facial paralysis brought on by Bell’s Palsy. For over the past 10 years, we have developed three-dimensional approaches to assess facial and circumoral soft tissue movements applied to patients with craniofacial deformities/disorders.
Patients born with cleft lip/palate may undergo numerous and extensive soft tissue surgeries in an attempt to normalize the facial features. Residual scarring as a result of these surgeries limits the optimum esthetic results. Our research indicates that patients remain with significant impairments in circumoral movement and disfigurement of the region. The dynamic and static objective measures that we have developed provide surgeons with a tool to more accurately assess both the extent of the impairment and degree of disfigurement, and ultimately, tailor revision surgeries to a patient’s individual needs.
What We Do
-

A movement analysis system, Motion AnalysisTM is made up of 8 Kestrel cameras, positioned at different viewpoints in order to capture all angles and curvatures of a patient’s face. Using a marker placement template or reference photograph, Facial Animation Laboratory staff apply 3 millimeter reflective markers, circular shaped hemispheres, to participants’ faces using eyelash adhesive or double adhesive tape. The animations patients are instructed to make include movements such as lip purse, cheek puff, maximum smile, mouth open, grimace, and natural smile.
-
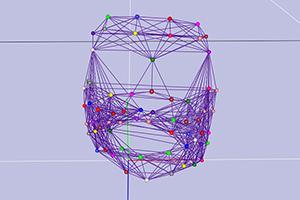
Once data is collected from patients on the Motion AnalysisTM system, research staff tracks the data. The color-coded points correspond with 64 different reflective markers that are placed on the subject’s face. The 8 Kestrel cameras locate and track each individual marker from their respective vantage points and converge the images into one three-dimensional image, shown here. Researchers can manipulate the image, zooming in/out and rotating the face to evaluate all angles, and also measure the distances each marker travels when the subject performs various facial animations. In this picture, a subject with unilateral left-side facial paralysis is demonstrating a maximum smile.
-

The 3dMDTM Static camera system captures three-dimensional still photographic images of patients in peak positions of each movement.
-

Three video camcorders are positioned to record the frontal and both profile views of the patient’s face simultaneously. The participant’s face fills each camera view on the video monitor, allowing researchers to view the participant’s face from all angles simultaneously on one screen. The participant is instructed to make different animations using a randomized sequence that include lip purse, cheek puff, maximum smile, mouth open, grimace, and natural smile.
-

The Team
Carroll Ann Trotman, BDS, MA, MS
Principal Investigator
Dr. Trotman is Professor and Chair and Program Director of the Orthodontic Department at Tufts University School of Dental Medicine and Adjunct Professor at the University of North Carolina School of Dentistry. She is the founder of the Facial Animation Laboratory at Tufts University. Her leading-edge work and innovative concepts in craniofacial translational research has advanced research forward towards innovative approaches in orthodontics. Dr. Trotman received her dental degree from Dundee University, Scotland and her Orthodontic Degree and MA in Oral Biology from Columbia University, NY. She then completed a Fellowship in Craniofacial Anomalies at the Hospital for Sick Children in Toronto. She has an MS in Clinical Research Design and Statistical Analysis from the Horace Rackham School of Graduate Studies, was an American Council on Education Fellow, is a Diplomate of the American Board of Orthodontics, and maintains and active research program with a focus on craniofacial anomalies.
Dr. Trotman has broad expertise in the treatment and care of patients with Cleft Lip/Palate and craniofacial anomalies, with specific training in clinical research and statistical analyses. As a faculty member at both the University of North Carolina at Chapel Hill and Tufts University School of Dental Medicine, she has served and is currently serving as Principal Investigator on NIH-funded grants, all of which are related to, and served as the precursor for, the current research described on this site. Dr. Trotman has laid the groundwork for this current research by developing novel quantitative and objective measures to assess facial disability – measures that are applicable to all craniofacial patients.
Ceib Phillips, PhD, MPH
Co-Investigator
Dr. Phillips is Professor and Interim Chair of Orthodontics in the UNC-Chap Hill School of Dentistry. She received her doctorate from the University of Wisconsin and her Master of Public Health degree in Biostatistics from UNC-Chapel Hill. She joined the University’s faculty in 1978. Phillips is a recognized leader in clinical research related to orthodontic and oral and maxillofacial surgery treatments with a focus on patient recovery and patient perception of process and outcomes. Her teaching responsibilities are primarily within the Department of Orthodontics and the research core of the postdoctoral program.
Dr. Phillips has a broad background in prospective, observational clinical studies as well as clinical trials with specific training and expertise in the quantitative statistical methodologies applicable to the ongoing facial animation research projects. Her own research focus over the last ten years has been on assessing patient recovery following surgery including patient self-report, neurosensory assessments, and physical well-being.
Julian Faraway, PhD
Co-Investigator
Dr. Faraway has sixteen years of experience working on the analysis of functional data. He has developed new methods for the analysis of facial animation data, and has published literature in both biomechanics and orthodontics demonstrating the applications of the methods that he has developed. Dr. Faraway has extensive experience in the analysis of motion capture dating back to his position at the University of Michigan where he served as Associate Director of the Human Motion Simulation laboratory and as a collaborator with Dr. Carroll-Ann Trotman when she worked at the School of Dentistry at the University of Michigan collecting facial motion capture data. Dr. Faraway has continued to collaborate with Dr. Trotman, in addition to analyzing motion capture data from Sports Science and Psychiatry.
Dr. Faraway’s skills lie in the development of statistical theory for data taking the form of curves and shapes and in the computing ability to apply these methods to data that often requires substantial and complex processing. This combination of skills is unusual and allows him to form an effective bridge between statistical theory and practice for the type of data collected in Dr. Trotman’s Facial Animation Laboratory.
M. Elizabeth (Betsy) Bennett, PhD
Co-Investigator
A major goal of the U-award grant research is to qualitatively explore how surgeons integrate a new assessment tool (The Intervention) into their decision-making processes before, during, and after surgery. Because of Dr. Bennett’s experience in both academic settings and medical market research, she is uniquely qualified to conduct interviews with surgeons and guide the qualitative analysis of the resultant data. Specifically, she has been an instructor and researcher in dentistry for over 20 years, and has worked in medical market research/consulting since 1998. In both roles, Dr. Bennett has explored how physicians and dentists make decisions about new products and/or services, and how they eventually incorporate new technologies into practice (or not, as the case may be).
Dr. Bennett’s work has spanned the qualitative-quantitative continuum, and she has published work that utilizes these methodologies in dentistry. In summary, her experience across a wide spectrum of providers (including surgeons), patients (including CL/P), and settings (corporate and academic) has prepared Dr. Bennett to direct this component of the proposed research.
Ashley Corrado
Project Administrator
Ashley joined the Facial Animation Laboratory team in August 2019. She is responsible for overall management of the laboratory at Tufts University. Her responsibilities include all aspects of coordinating a clinical trial and implementing research protocols. This includes recruitment of subjects, data collection, and data processing, in addition to acting as liaison between investigators and the Tufts University Health Sciences Institutional Review Board (IRB), Massachusetts General Hospital IRB, and Boston Children’s Hospital IRB. Ashley is the primary contact for all research participants, surgeons and collaborators from the institutions listed above, and also for any inquiries from participating Review Boards.
Eli Maayan
Research Coordinator
Eli joined the Facial Animation Laboratory team as a Research Coordinator in June 2019. He works closely with Dr. Trotman and the Project Administrator to handle patient recruitment activities, data collection and processing, as well as develop and manage subject databases for ongoing studies. He also oversees the technical aspects of the lab to ensure that the equipment runs smoothly during the study visit and that the data collected is adequately stored afterwards.
Ashwini Joshi
Clinical Research Specialist at University of North Carolina Facial Animation Laboratory
Ashwini joined the Facial Animation Laboratory in January 2019. She is responsible for all day to day laboratory activities: recruiting subjects, collecting and processing facial animation data preparing intervention media with processed stills, videos, and tracking data, training surgeons in the use of the intervention media, maintaining the facilities, equipment, and supervising/training work-study and volunteer research assistants. As a research specialist at the UNC site, she is the primary contact for subjects and surgeons at UNC and Wake Forest University, and collaborates with the research team at Tufts University with regard to project meetings, Manual of Operations, and publication presentation. Visit the University of North Carolina Facial Animation Laboratory site here.
-
U01 Award
Targeting Surgeons’ Decision-Making for Lip Revision Surgery Cleft lip/palate (CL/P) are among the most common of all birth defects. To correct the obvious facial disabilities of babies with CL/P, surgeons perform an initial or primary repair of the lip and nose soon after birth. Unfortunately, many patients (and caregivers) are dissatisfied with the surgical results: Patients remain with a facial disfigurement and impairment in facial soft tissue movements—particularly in facial expressive behaviors. Multiple revision surgeries during childhood and adolescence are common to improve the initial results. The psychosocial and economic burden of care on these children and their caregivers are great. Traditionally, the decision for lip revision surgery has been based on subjective assessments of nasolabial form, and less frequently, circumoral movement but without a method to quantify the facial movements/form before surgery or after surgery. To this end, we have developed an Intervention that utilizes a novel set of dynamic and static quantitative measures and a systematic subjective evaluation to quantify facial disability for the treatment planning of lip surgery and for assessing surgical outcomes. The quantitative measures include (1) 3D dynamic and statistical modeling of patients’ mean facial movements and (2) 3D static facial image data, both compared with mean control movement and static image data, respectively. As a necessary second step in this formative research, using separate prospective cohorts of patients who have lip revision and lip repair surgery, we will conduct a ‘proof of concept’ Phase II randomized clinical trial (RCT) with the following Specific Aims.
Specific Aim 1. To qualitatively assess how surgeons integrate the Intervention’s objective measures and visual aids with the systematic subjective assessment in the decision-making process for the clinical surgical procedures of lip revision and lip repair.
Specific Aim 2. To quantitatively assess the extent to which the Intervention changes surgeons’ problem list and treatment planning goals for lip revision and lip repair.
Specific Aim 3. To obtain estimates on means, variances, and intra-patient correlation, and to estimate surgeon-by-condition interaction effects for surgical outcomes under the Intervention and the standard of care or Control conditions.
Ultimately, while this Phase II RCT is not a therapeutic trial in the usual sense of providing a patient with a therapy, it will be unique for craniofacial rehabilitation in that the focus is to optimize the design of a novel assessment, improve an individual patient’s diagnostic evidence base available to the surgeon for surgical planning, and evaluate whether post-surgical results are improved with the Intervention.
Collaborating Investigators on the U01 grant:
- Carroll Ann Trotman, BDS, MA, MS - Tufts University School of Dental Medicine
- William Austen, MD - Massachusetts General Hospital
- Eric Liao, MD, PhD - Massachusetts General Hospital
- Carolyn Rogers-Vizena, MD - Boston Children’s Hospital
- Ingrid Ganske, MD - Boston Children’s Hospital
- Jehan Wood, MD - University of North Carolina, Chapel Hill
- Renie Daniel, DMD, MD - University of North Carolina, Chapel Hill
- Lisa David, MD - Wake Forest University
Other Key Personnel:
- Ceib Phillips, PhD, MPH - University of North Carolina, Chapel Hill
- Richard Bruun, DDS - Boston Children’s Hospital
- Julian Faraway, PhD - University of Bath, United Kingdom
- Elizabeth Bennett, PhD - Clarity Consulting
R21 Award
Function and Form Outcomes in Patients with Facial Paralysis
Patients with facial paralysis have an obvious facial disability. The resultant facial disability includes facial disfigurement and impairment in soft tissue movements, particularly in facial expressive behaviors. These negative physical sequelae not only impact facial esthetics and function, but also patients’ social and emotional quality of life. Treatments range from nonsurgical interventions and facial reanimation surgery to new implantable facial pacing devices that would potentially initiate artificial movement on the paralyzed side of the face. Traditionally, surgeons’ plan treatment based on isolated measurements made from 2D photographs and subjective grading of the patient’s face, both of which are limited in scope and dimension. Our research group has demonstrated the utility of novel 3D dynamic and static quantitative (objective) measures for the evaluation of facial soft tissue function (NIH DE 013814, DE 016964, and DE 013814- 08S1). These measures have been validated for use in the cleft lip/palate (CL/P) patient population. The measures are objective and quantitative, and they provide a more precise diagnosis of facial soft tissue disability and evaluation of surgical outcomes. The main goal of this prospective, observational study is to determine the applicability of these novel 3D dynamic and static measures for quantification and measurement of impairment and disfigurement, as well as change over time, in patients with facial paralysis. The global hypothesis is that the use of the measures will provide a more comprehensive analysis of the severity of facial paralysis and the changes over time (recovery) when compared with current assessment methods. The specific aims of the study are as follows:
- Specific Aim 1. To quantitatively evaluate the range of facial soft tissue disability (facial impairment and disfigurement) in patients with acute, unilateral, flaccid facial paralysis and track the changes over time (3-month recovery period) and to compare the facial disability in the patients with a group of age- and sex-frequency matched normal subjects.
- Specific Aim 2. In patients with acute, unilateral, flaccid facial paralysis, to compare the current, qualitative, clinical assessment methods for facial impairment and disfigurement (House-Brackman Facial Nerve Grading System & Sunnybrook Facial Grading System) with the objective quantitative assessments in order to assess the differential information provided by a quantitative zonal analysis versus a qualitative global assessment.
- Specific Aim 3. (a) To assess perceptions of facial appearance and quality of life over time in patients with acute, unilateral, flaccid facial paralysis and to compare these perceptions with those of control subjects, and (b) To correlate the patients’ perceptions over time with the quantitative measures of facial disability.
Ultimately, this study is unique for the rehabilitation of patients with facial paralysis in that the focus is on generating novel, objective, 3D measures to characterize the condition and temporal changes, and on the generation of future hypotheses to optimize interventions and assess the outcomes of the different treatments.
-
Please find a selection of Dr. Trotman’s publications relevant to her current research listed below:
- Trotman, C.-A., Faraway, J.J., Soltmann, R., Hartman, T., vanAalst, J. Facial soft tissue dynamics before and after primary lip repair. Cleft Palate-Craniofac. J. 50(3):315-322, 2013. PMID:23050657
- Trotman, C.-A., Phillips, C., Faraway, J.J., Hartman, T., vanAalst J.A. Influence of objective three dimensional measures and movement images on surgeon treatment planning for lip revision surgery. Cleft Palate-Craniofac. J. 50(6):684-95, 2013. PMID: 23855676. PMCID: PMC3830636.
- Mercado, A.M., Phillips, C., Vig, K.W.L., Trotman, C.-A. Effects of lip revision surgery on nasolabial esthetics in patients with cleft lip. & Craniofac. Res. Submitted Feb, 2013.
- Barlow, S.M., Trotman, C.-A., Chu, S.Y., Lee, J. Modification of perioral stiffness in children with repaired cleft lip and palate. Cleft Palate-Craniofac J. 49(5):524-529, 2012. PMID:21247345.
- . Essick, G., Phillips, C., Chung, Y., Trotman, C.-A. Effects of lip revision surgery on long-term orosensory function in patients with cleft lip/palate. Cleft Palate-Craniofac. J. 2012. [Epub ahead of print]. PMID:22906391.
- Faraway, J.J. and Trotman, C.-A. Shape change along geodesics with application to cleft lip surgery. Royal Stat. Society Appl. Statist. 60(5):743-755, 2011. PMID:22639469. PMCID:PMC3359093.
- Trotman, C.-A. Faces in 4D—Why do we care and why the 4th dimension? J. Ortho. Dentofac. Orthop. Am. J. Ortho. Dentofac. Orthop. 140(6):895-899, 2011. PMID:22133956. PMCID:PMC3387984.
- Tanikawa, C., Takada, K., van Aalst, J., Trotman, C.-A. Objective 3D assessment of lip form in patients with repaired cleft lip. Cleft Palate-Craniofac. J. 47(6):611-622, 2010. PMID:20500076. PMCID:PMC2970757.
- Trotman, C.-A., Faraway, J.J., Phillips, C., van Aalst, J. Effects of Lip Revision Surgery in Cleft Lip/Palate Patients. Dent. Res. 89(7):728-732, 2010. PMID:20439935. PMCID:PMC2967701.
- Trotman, C.-A., Faraway, J.J. Smile analysis and quantification. In Silico Dentistry—the evolution of computational oral health science. Takada, K. & Kreiborg, S. Medigit, Osaka, Pgs. 68-70, 2008.
- Trotman, C.-A., Faraway, J.J., Losken, H.W., van Aalst, J. Functional outcomes of cleft lip surgery. Part II: Quantification of nasolabial movement. Cleft Palate-Craniofac. J. 44:607-616, 2007. PMID:18177193.
- Trotman, C.-A., Phillips, C., Essick, G.K., Faraway, J.J., Barlow, S.M., Losken, H.W., van Aalst, J., Rogers, L. Functional outcomes of cleft lip surgery. Part I: Study design and surgeon ratings of lip disability and the need for lip revision. Cleft Palate-Craniofac. J. 44:598-606, 2007. PMID:18177192.
- Trotman, C.-A., Barlow, S.M., Faraway, J.J. Functional outcomes of cleft lip surgery. Part III: Measurement of lip forces. Cleft Palate-Craniofac. J. 44:617-623, 2007. PMID:18177195.
- Essick, G.K., Phillips, C., Trotman, C.-A. Functional outcomes of cleft lip surgery. Part IV: Factors affecting lip vermillion sensory thresholds. Cleft Palate-Craniofac. J. 44:624-634, 2007. PMID:18177194.
- Trotman, C.-A., Faraway, J.J., Phillips, C. Visual and statistical modeling of facial movement in patients with cleft lip. Cleft Palate-Craniofac. J. 42:245-254, 2005. PMID:18565457.
- Essick, G.K., Dorion, C., Rumley, S., Rogers, L., Young, M., Trotman, C.-A. Report of altered sensation in patients with cleft lip. Cleft Palate-Craniofac. J. 42:178-184, 2005. PMID:15748109.
- Lee, J.Y., Han, Q., Trotman, C.-A. Three-dimensional facial imaging: Accuracy and considerations for clinical applications in orthodontics. Angle Orthod. 74:587-593, 2004. PMID:15529491.
- Trotman, C.-A., Faraway, J.J. Modelling facial movement: I. A dynamic analysis of differences based on skeletal characteristics. In Press J. Oral Maxillofac. Surg. 62:1372- 1379, 2004. PMID:15510358.
- Nooreyazdan, M., Trotman, C.-A., Faraway, J.J. Modelling facial movement: II. A dynamic analysis of differences due to orthognathic surgery. Oral Maxillofac. Surg. 62:1380-1386, 2004. PMID:15510359.
- Trotman, C.-A., Phillips, C., Faraway, J.J., Ritter, K. Association between subjective and objective measures of lip form and function: An exploratory analysis. Cleft Palate Craniofac. J. 40:241-248, 2003. PMID:12733951.
- Ritter, K., Trotman, C.-A., Phillips, C. Validity of subjective evaluations for the assessment of lip scarring and impairment. Cleft Palate Craniofac. J. 39:587-596, 2002. PMID:12401105.
- Weeden, C., Trotman, C.-A., Faraway, J.J. Three-dimensional analysis of facial movement in normal adults: Influence of sex and facial shape. Angle Orthod. 71:132- 140, 2001.
- Trotman, C.-A., Faraway, J.J, Essick, G.K.. 3-D Nasolabial displacement during movement in repaired cleft lip and palate patients. J. Plastic & Reconstr. Surg. 105:1273- 1283, 2000. PMID:10744215.
- Trotman, C.-A., Stohler, C.S., Johnston, L.E., Jr. Measurement of facial soft tissue mobility in man. Cleft Palate Craniofac. J. 35:16-25, 1998.
- Trotman, C.-A., Faraway, J.J., Silvester, K.T., Greenlee, G.M., Johnston, L.E., Jr. Sensitivity of a method for the analysis of facial mobility: Vector of displacement. Cleft Palate Craniofac. J. 35:132-141, 1998.
- Trotman, C.-A., Faraway, J.J. Sensitivity of a method for the analysis of facial mobility: Inter-landmark separation. Cleft Palate Craniofac. J. 35:142-153, 1998.
- Trotman, C.-A., Gross, M.M., Moffatt, K. Reliability of a three-dimensional method for measuring facial animation: A case report. Angle Orthod. 66:195-198, 1996.
- Gross, M.M., Trotman, C.-A., Moffatt, K.S. A comparison of three-dimensional and two-dimensional analyses of facial motion. Angle Orthod. 66:189-194, 1996.